Research on the use of urine biomarkers for early detection of pancreatic cancer
Q&A with Professor Tatjana Crnogorac-Jurcevic and Dr Silvana Debernardi
November is Pancreatic Cancer Awareness Month. There are approximately 10,500 new cases of pancreatic cancer diagnosed in the UK each year. A lack of specific symptoms in the early stages of the disease mean that pancreatic cancer is often diagnosed at an advanced stage when treatment is less likely to be successful. In England, only about 7% of people with pancreatic cancer will live for 5 years or more beyond their diagnosis. Early detection of pancreatic cancer is vital to improve outcomes for patients.
Professor Tatjana Crnogorac-Jurcevic and her team at Barts Cancer Institute, Queen Mary University of London, are working to identify biological clues or ‘biomarkers’ for early, non-invasive detection of pancreatic cancer in urine samples. In their most recent paper, published in the International Journal of Cancer, the team reported that a urine biomarker panel could detect pancreatic ductal adenocarcinoma (PDAC), the most common type of pancreatic cancer, up to 2 years before clinical diagnosis.
We spoke to Professor Crnogorac-Jurcevic and postdoctoral researcher Dr Silvana Debernardi, who is first author of the paper, to find out more about the research.
What is your new study about and what did you find?
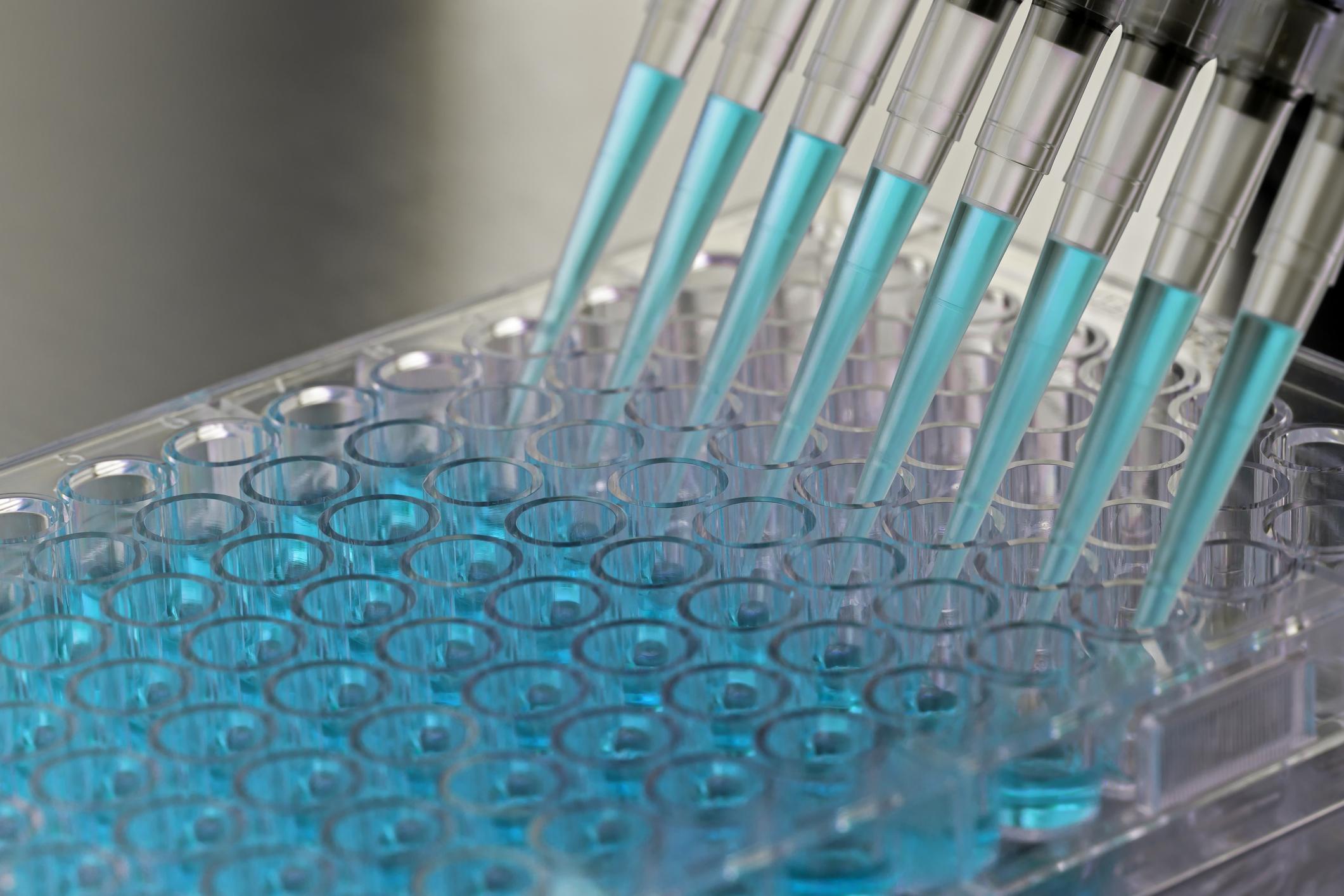
In this new study, we analysed our previously reported biomarker panel for earlier detection of pancreatic cancer in prediagnostic urine samples. We measured the biomarker levels in urine samples from 99 patients with PDAC that were prospectively collected up to 5 years prior to diagnosis, and in 198 matched control specimens from individuals without PDAC.
We show that our biomarkers can detect PDAC up to 2 years before clinical diagnosis, and their accuracy is enhanced when combined with the measurement of CA19-9 (a blood protein used as a pancreatic cancer marker in clinical practice). Using our previously developed algorithm, called PancRISK, we can discriminate pancreatic cancer from controls in 89% and 77% of cases, 12 and 24 months before diagnosis, respectively.
The urine samples were obtained from three pre-existing study cohorts: Shanghai Women’s Health Study (SWHS), the Shanghai Men’s Health Studies (SMHS) and the Southern Community Cohort Study (SCCS). All of the samples had been collected along with data on demographic factors, diet, lifestyle habits and medical history for each patient.
We also evaluated the predictive performance of the urinary panel in combination with epidemiological data, including known lifestyle risk factors (smoking, obesity and heavy alcohol use) as well as comorbidities, and observed that the addition of body mass index information improved the model performance.
What is the urine biomarker panel? How does it work?
The biomarker panel is composed of three proteins: LYVE1, REG1B and TFF1. These were selected from our previous analysis of proteins found in the urine of healthy controls, chronic pancreatitis and PDAC patients as being able to discriminate well between the different experimental groups. They were subsequently further validated in a multicentre cohort of 590 urine samples showing the ability, when combined into a panel, to distinguish control individuals and patients with benign hepatobiliary diseases from patients with early stage PDAC, with specificity and sensitivity of more than 85%.
For the analysis and interpretation of the data, we developed an algorithm called the PancRISK score, which, using the level of the biomarkers in urine in combination with a patient’s age, enables the stratification of patients into those with ‘normal’ or ‘elevated’ risk for developing PDAC.
How is pancreatic cancer currently detected in the clinic?
Symptoms of pancreatic cancer are not specific and appear late when the tumour is already locally advanced or has spread to other organs; it is usually diagnosed using imaging. Currently, no biomarkers for earlier detection of PDAC exist. The most commonly used biomarker in clinical practice, serum CA19-9, is not specific or sensitive enough for screening purposes when used alone - it is mainly used as a prognostic marker and for monitoring of treatment response.
What are your next steps for this research? How could urine testing for pancreatic cancer help in clinical practice?
We are currently performing the clinical validation of these urinary biomarkers in a prospective observational trial, called the UroPanc trial. Urine and blood samples are being collected from symptomatic patients with suspected pancreatic cancer, and asymptomatic individuals at high risk of developing PDAC due to family history and genetic background. In total, over 2,000 participants will be included in the study.
The urine biomarkers, alone or in combination with CA19-9, will be compared to imaging and, where available, data from microscope examinations of tissue samples. This will enable us to establish the accuracy of PancRISK to stratify the patients - only the ones with ‘elevated’ risk for developing PDAC will need to undergo further, usually invasive and expensive, clinical investigation, which will hopefully enable earlier detection of pancreatic cancer.
If successful, this patient stratification approach will be implemented into clinical practice, with the potential to significantly improve the current diagnostic pathway for pancreatic cancer patients.
Further information
- The research was funded by Cancer Research UK and the National Institute of Health
- Research paper: Urine biomarkers enable pancreatic cancer detection up to 2 years before diagnosis. Int J Cancer. 2022; 1- 12. doi:1002/ijc.34287
- Find out more about the UroPanc trial.
Category: General News, Interviews, Publications

No comments yet